In the dynamic realm of prehospital medicine, advancements in treatment modalities play a pivotal role in improving patient outcomes. One such innovation that has garnered attention is the use of tranexamic acid (TXA) in the prehospital setting.
Contrary to popular belief, TXA does not form clots; instead, it acts as an inhibitor, preventing the breakdown of clots, making it a valuable tool in managing traumatic injuries. TXA’s mechanism of action involves inhibiting fibrinolysis, the process by which clots are broken down. By preserving these clots, TXA contributes to the stabilization of bleeding and promotes hemostasis. This unique characteristic proves particularly advantageous in the prehospital setting, where rapid interventions are crucial.
One of the primary benefits of TXA lies in its ability to mitigate hyperfibrinolysis, a common complication in trauma cases. Trauma-induced coagulopathy often results in excessive clot breakdown, leading to uncontrolled bleeding. Administering TXA early in the prehospital phase helps address this issue, preventing the premature dissolution of clots and promoting a more stable hemostatic environment. The administration of TXA in the prehospital setting is a carefully orchestrated process. Emergency medical service (EMS) providers are trained to recognize potential candidates for TXA administration, such as patients with significant traumatic injuries or those at risk of hemorrhage. The timing of administration is critical, and early intervention can significantly impact outcomes.
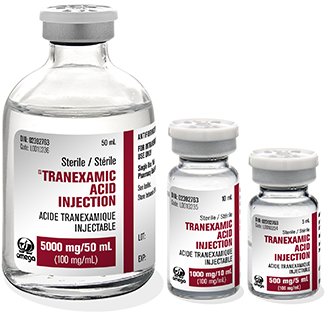
TXA is typically administered intravenously, with recommended doses ranging from 1 to 2 grams. This should be initiated as soon as possible after injury and continued during the hospital phase of care. The challenge lies in striking a balance between early administration and avoiding unnecessary use in patients without indications for TXA. Several studies have demonstrated the efficacy of TXA in reducing mortality and the need for blood transfusions in trauma patients. The landmark CRASH-2 trial highlighted the potential life-saving benefits of TXA, reinforcing its role in the management of traumatic hemorrhage. In the prehospital setting, where time is of the essence, these findings underscore the significance of timely TXA administration.
While TXA has shown promise, its use in the prehospital setting is not without considerations. In the context of pregnant women in the third trimester (greater than 24 weeks pregnant) with the fundus presenting above the umbilicus, the use of TXA needs to be carefully evaluated, and it is generally contraindicated. Here are some considerations:
- Risk to the Fetus: Limited data are available on the safety of TXA use during pregnancy, particularly in the third trimester. There is concern that TXA may cross the placenta, potentially affecting the fetus.
- Uterine Contraction Effects: TXA could theoretically affect uterine contractions. In late pregnancy, uterine contractions are crucial for the well-being of the fetus, and any interference with these contractions could be problematic.
- Potential for Thromboembolism: Pregnant women are already at an increased risk of thromboembolic events. TXA may potentially increase this risk further.
- Maternal Health: The overall health of the pregnant woman should be considered, including any pre-existing conditions or medical history that might contraindicate the use of TXA.
In saying that it is generally considered safe for use in cases of postpartum hemorrhage.
Careful patient selection, ongoing research, and continued training for EMS providers are essential to optimize its benefits. Moreover, the integration of TXA into prehospital protocols necessitates collaboration between emergency medical services and hospitals to ensure seamless care transitions.
In conclusion, the use of tranexamic acid in the prehospital setting represents a significant stride in trauma care. Its ability to preserve clots and mitigate hyperfibrinolysis addresses a critical aspect of traumatic hemorrhage management. As research advances and protocols evolve, the strategic administration of TXA holds the potential to save lives and redefine standards of care in the challenging landscape of prehospital medicine.