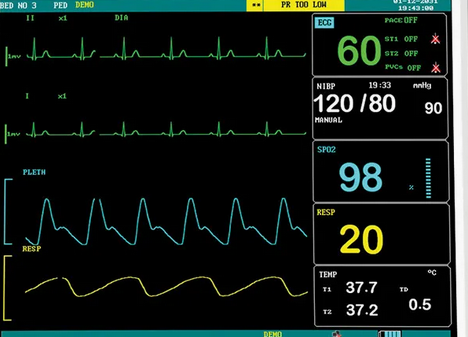
In both ICU and pre-hospital settings, non-invasive blood pressure (NIBP) monitoring has become a cornerstone of patient management. However, a common and concerning practice has emerged: using NIBP-derived systolic and diastolic pressures to calculate the mean arterial pressure (MAP) for titration of blood pressure medications. This practice, while widespread, can lead to inaccuracies due to the limitations of NIBP technology and the reliance on algorithmically generated values [1][2].
Understanding Blood Pressure Measurement: The Korotkoff Method
Before addressing the limitations of NIBP, it’s important to understand the traditional auscultation method of measuring blood pressure. The Korotkoff method involves using a sphygmomanometer and a stethoscope to detect the sounds of blood flow, known as Korotkoff sounds, as the cuff pressure is released [3].
- Systolic Pressure: The pressure at which the first Korotkoff sound is heard, indicating the onset of blood flow through the compressed artery [3].
- Diastolic Pressure: The pressure at which the Korotkoff sounds disappear, indicating unimpeded blood flow [3].
The MAP in this context is calculated using the formula:
MAP=Diastolic Pressure+(Systolic Pressure−Diastolic Pressure)3\text{MAP} = \text{Diastolic Pressure} + \frac{(\text{Systolic Pressure} – \text{Diastolic Pressure})}{3}
This method provides accurate systolic and diastolic values that can reliably be used to calculate MAP [4].
How NIBP Devices Measure Blood Pressure
NIBP monitors, commonly used in ICUs and pre-hospital settings, use the oscillometric method rather than auscultation. This method measures the oscillations of arterial wall vibrations caused by blood flow as the cuff inflates and deflates [5][6].
- MAP Accuracy: The MAP is the most accurate value obtained by oscillometric devices because it corresponds to the point of maximum oscillations [5][6].
- Algorithm-Generated Systolic and Diastolic Pressures: Unlike MAP, systolic and diastolic pressures are not directly measured. They are derived using proprietary algorithms based on the shape and amplitude of the oscillation curve [6].
The Problem with Using NIBP-Derived Systolic and Diastolic Pressures
Many clinicians use the systolic and diastolic pressures from NIBP devices to calculate MAP manually. However, this approach is flawed because:
- Algorithmic Variability: The algorithms used by NIBP devices to estimate systolic and diastolic pressures are manufacturer-specific and not universally standardized. This variability can lead to inconsistent and inaccurate readings [6][7].
- Inaccuracy of Derived Pressures: The algorithmically generated systolic and diastolic pressures may not accurately reflect the patient’s true blood pressure, especially in cases of arrhythmias, hypotension, or vasoconstriction [5][7].
- Compounding Error: When these potentially inaccurate values are used to calculate MAP, the resulting value may deviate significantly from the actual MAP [5][6][7].
The Importance of Using NIBP-Generated MAP
The MAP generated by NIBP devices is far more reliable because it is based directly on the oscillometric measurements. Studies have shown that MAP obtained in this way closely correlates with invasive arterial pressure monitoring, making it a trustworthy parameter for clinical decision-making [6][7][8].
Key Takeaways for Best Practices
- Rely on MAP from NIBP Devices: Use the MAP displayed on the monitor, as this value is derived from the most accurate aspect of the oscillometric method [6][8].
- Avoid Calculating MAP from Systolic and Diastolic Pressures: Do not use NIBP-derived systolic and diastolic pressures to manually calculate MAP, as this introduces unnecessary inaccuracies [5][7].
- Educate Clinical Teams: Ensure that clinicians understand the limitations of NIBP technology and the significance of relying on MAP over derived pressures for titration of medications [8].
- Confirm with Invasive Monitoring if Needed: In critical scenarios, confirm NIBP readings with invasive arterial pressure monitoring to ensure accuracy [6].
Conclusion
While NIBP devices are invaluable tools in ICU and pre-hospital care, their limitations must be understood to avoid potential pitfalls. The practice of using NIBP-derived systolic and diastolic pressures to calculate MAP can lead to errors in patient management, particularly when titrating blood pressure medications. By focusing on the NIBP-generated MAP, clinicians can make more accurate and effective treatment decisions, ultimately improving patient outcomes. Accurate blood pressure monitoring is not just a technical detail—it is a cornerstone of safe and effective care [5][6][8].
References
- Pickering, T. G., et al. (2005). Recommendations for blood pressure measurement in humans and experimental animals: Part 1: Blood pressure measurement in humans. Hypertension, 45(1), 142-161.
- Parati, G., et al. (2003). Blood pressure variability: Its measurement and significance in hypertension. Journal of Hypertension, 21(12), 2211-2223.
- Korotkoff, N. (1905). On the subject of methods of studying blood pressure. Bulletin of Imperial Military Medical Academy, 11, 365-367.
- Guyton, A. C., & Hall, J. E. (2021). Textbook of Medical Physiology. Elsevier Health Sciences.
- Mancia, G., & Grassi, G. (2014). The oscillometric blood pressure measurement method: Evidence and uncertainties. Journal of Hypertension, 32(3), 481-484.
- Omboni, S., et al. (2015). Accuracy of oscillometric blood pressure measurement devices. Hypertension Research, 38(8), 570-575.
- O’Brien, E., et al. (2013). Blood pressure measuring devices: Recommendations for clinical validation. European Society of Hypertension.
- Drummond, J. C. (2019). Blood pressure measurement: What the anesthesiologist should know. Anesthesia & Analgesia, 128(5), 1246-1253.