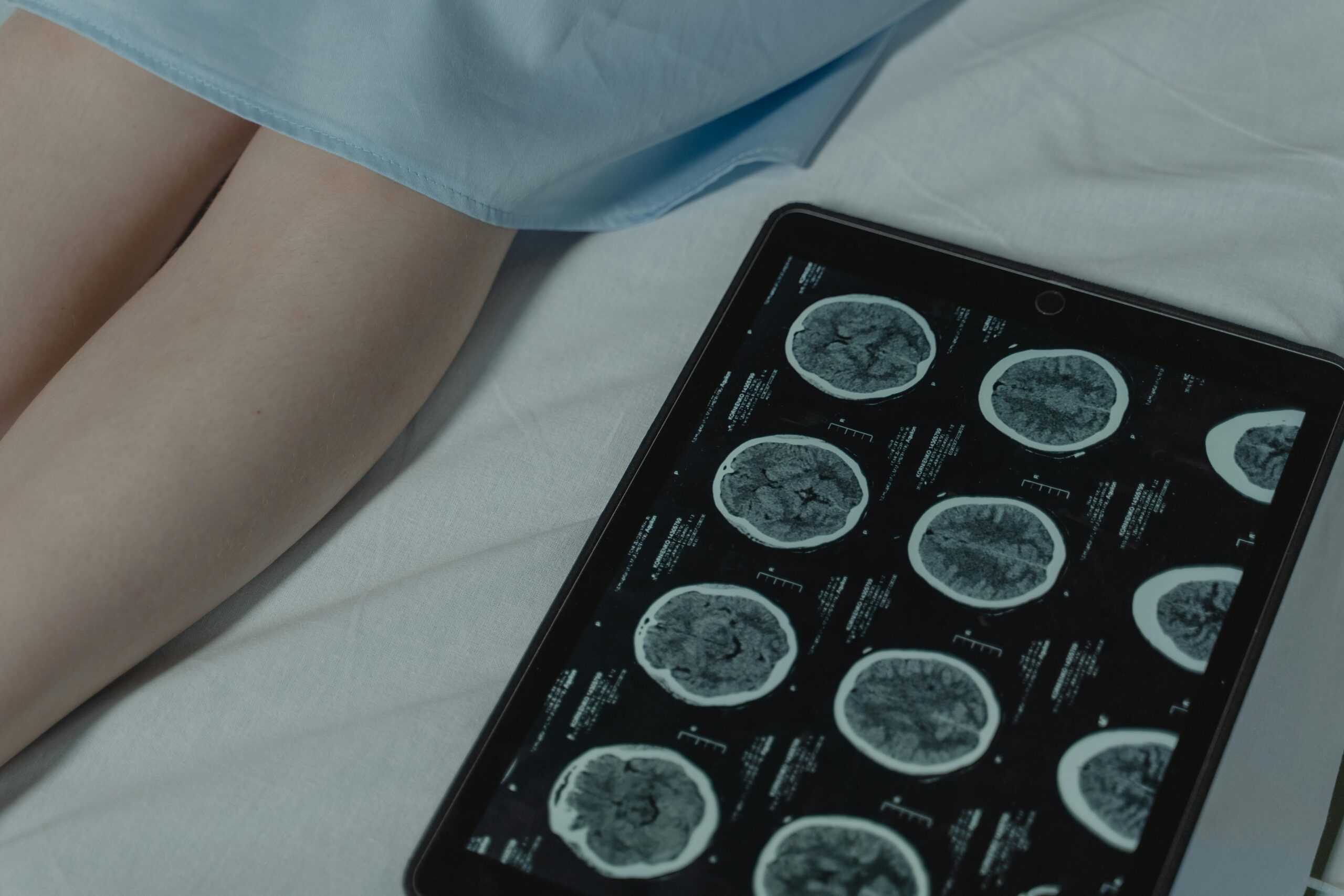
In the realm of healthcare, intra-facility patient transfers, especially via medevac flights, demand meticulous planning and adherence to safety protocols. When dealing with patients requiring External Ventricular Drainage (EVD), such transfers present unique challenges that necessitate careful consideration to avoid potential complications. Understanding the intricacies of EVD management and the repercussions of overlooking critical protocols like clamping the EVD during transfers is paramount to ensuring patient safety and well-being.
Navigating the Complexities of EVD Management During Transfers:
External Ventricular Drainage (EVD) plays a crucial role in managing patients with various neurological conditions, necessitating precise fluid management and intracranial pressure (ICP) regulation. However, during intra-facility transfers, particularly via medevac flights, maintaining this delicate balance becomes even more challenging.
Understanding the relationship between the Zero and EVD levels.
The relationship between the zero level, typically the level of the tragus (the small, pointed projection in front of the external opening of the ear), and the height of an External Ventricular Drainage (EVD) system above this zero level is crucial for accurate measurement and regulation of intracranial pressure (ICP).
The zero level, or the level of the tragus, serves as a reference point for measuring the height of the EVD system above the patient’s head. The EVD system consists of a drainage catheter inserted into the ventricular system of the brain, connected to an external drainage system. The height of the EVD system above the zero level determines the pressure within the system, as it relates to gravity and the weight of the column of cerebrospinal fluid (CSF) within the drainage catheter.
The height of the EVD system above the zero level affects the pressure within the system according to the principles of hydrostatic pressure. As the EVD system is raised above the zero level, the pressure within the system decreases, and vice versa. This relationship is crucial in regulating the drainage of CSF and managing intracranial pressure in patients with neurological conditions such as hydrocephalus, traumatic brain injury, or intracranial hemorrhage.
Healthcare professionals adjust the height of the EVD system above the zero level based on the patient’s clinical condition and the desired level of CSF drainage. For example, lowering the EVD system below the zero level increases the pressure within the system, which can facilitate CSF drainage in patients with elevated intracranial pressure. Conversely, raising the EVD system above the zero level decreases the pressure, which may be necessary to reduce CSF drainage in patients with low ICP or to prevent over-drainage
The Impact of EVD Settings on CSF Drainage:
The amount of CSF drainage from an EVD is intricately linked to the pressure differential between the ICP and the height of the drainage chamber. Understanding this relationship is essential when considering the repercussions of not adhering to clamping protocols during transfers:
- Risk of Over-Drainage: Adjusting the patient’s position or transferring them without clamping the EVD can lead to a lowered threshold for CSF drainage. This poses a significant risk, especially during medevac flights where environmental factors and altitude changes can further exacerbate ICP dynamics.
Practical Considerations for Safe Patient Handling:
In the context of intra-facility transfers via medevac flights, several crucial considerations must be addressed to mitigate risks associated with EVD management:
- Pre-Transfer Planning: Prior to the transfer, healthcare teams must conduct a comprehensive assessment of the patient’s condition, including EVD settings and CSF drainage trends. Including how to mitigate potential complications which may arise. This information allows for critical clinical decisions making regarding EVD management during the transfer process.
- Strict Adherence to Clamping Protocols:It is imperative never to adjust the patient’s position or move them without first clamping the EVD. Considering that the daily production of CSF is equivalent to the volume of a standard soda can (approximately 300-600 mL), failure to do so can disrupt CSF drainage dynamics, and potentially lead to complications. Consistent over-drainage poses significant risks, including subdurals, hygromas, and even intracranial hypotension or upward herniation in specific cases.
- Continuous Monitoring During Transfer: Throughout the transfer process, vigilant monitoring of the patient’s vital signs, ICP levels (if possible), and EVD function is essential. Any deviations from expected parameters should prompt immediate intervention to mitigate potential risks.
Conclusion:
Intra-facility patient transfers via medevac flights present unique challenges, particularly when managing patients with EVDs. By understanding the intricacies of EVD management and adhering to strict protocols, healthcare teams can mitigate risks and ensure the safety and well-being of patients throughout the transfer process. Prioritizing meticulous planning, continuous monitoring, and adherence to safety protocols is paramount in achieving successful outcomes for patients requiring EVD management during intra-facility transfers.