Introduction
Mechanical ventilation is a critical life-saving intervention used in various medical settings to support patients who are unable to breathe adequately on their own. Central to its effectiveness are three fundamental parameters: Positive End-Expiratory Pressure (PEEP), Peak Inspiratory Pressure (PIP), and Plateau Pressure (Pplat). Understanding these parameters is essential for healthcare providers to ensure optimal patient outcomes [1].
The Normal Breathing Process
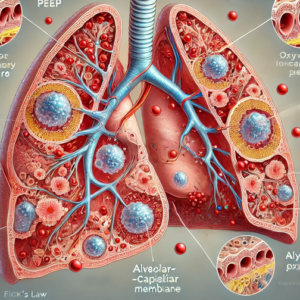
To appreciate the importance of these parameters, we need to understand the normal breathing process. During normal breathing, the diaphragm contracts and moves downward, creating negative pressure within the thoracic cavity. This negative pressure draws air into the lungs, inflating the alveoli where gas exchange occurs [2].
During expiration, the diaphragm relaxes, and the elastic recoil of the lungs pushes air out of the alveoli. But how exactly is positive pressure maintained within the alveoli during this process [3]?
How Intrinsic Pressures Are Maintained in the Alveoli
Let’s delve deeper into how the pressure is maintained within the alveoli during expiration. The key concept here is the role of elastic recoil and the slight positive pressure that persists in the alveoli at the end of expiration [4].
When the diaphragm relaxes during expiration, the lungs’ elastic tissues, which were stretched during inhalation, naturally recoil. This elastic recoil creates a force that helps push the air out of the alveoli and into the airways, eventually leaving the body through the nose or mouth. At the end of expiration, the pressure within the alveoli remains slightly positive. This positive pressure is mainly due to airway resistance and the intrapleural pressure, which acts as a mechanical barrier preventing the alveoli from collapsing completely [5]. This residual pressure ensures that a small volume of air, known as Functional Residual Capacity (FRC), is always present to prevent alveolar collapse and facilitate efficient gas exchange in subsequent breaths [6].
If the alveoli were to collapse, it would require significant effort to reopen them with each breath, leading to inefficient breathing and potential respiratory distress [7].
The Importance of PEEP
Positive End-Expiratory Pressure (PEEP) is the pressure applied by the ventilator at the end of expiration to keep the alveoli open. PEEP is vital because it:
- Prevents alveolar collapse (atelectasis) [8].
- Increases Functional Residual Capacity (FRC) [9].
- Improves oxygenation by keeping the alveoli open [10].
Without adequate PEEP, alveoli can collapse, reducing the surface area available for gas exchange and increasing the risk of ventilator-associated lung injury [11]. By maintaining appropriate PEEP levels, we ensure that the alveoli remain open, promoting better oxygenation and reducing the work of breathing for the patient [12].
Diminished Airway Resistance with Endotracheal Tube (ETT) Placement
When an endotracheal tube (ETT) is placed in the airway, it significantly reduces airway resistance. This is because the ETT provides a direct, unobstructed path for air to flow into the lungs, bypassing the natural anatomical structures that usually contribute to airway resistance [13]. However, while the ETT helps to ensure that the ventilated breaths are delivered efficiently, it also removes the body’s natural ability to maintain certain intrinsic pressures (Natural PEEP), underscoring the importance of correctly setting and monitoring PEEP [14].
Understanding PIP: Peak Inspiratory Pressure
Peak Inspiratory Pressure (PIP) is the maximum pressure reached during inspiration when the ventilator delivers a breath. This parameter is crucial for ensuring that the ventilated breath reaches the alveoli without causing barotrauma [15].
Normal Maximum Pressure
The normal maximum PIP is typically kept below 30-35 cmH2O to minimize the risk of lung injury. Exceeding this pressure can lead to overdistension of the alveoli, causing barotrauma and volutrauma, which can further compromise lung function [16].
Maintaining Safe PIP Levels
Healthcare providers must monitor PIP closely and adjust ventilator settings to keep pressures within safe limits. This involves ensuring that the tidal volume is appropriate for the patient’s lung compliance and that inspiratory flow rates are optimized [17].
The Role of Pplat: Plateau Pressure
Plateau Pressure (Pplat) is measured during a brief inspiratory hold maneuver and reflects the pressure applied to the small airways and alveoli when there is no airflow. Pplat is an important indicator of lung compliance [18].
Understanding Compliance
Lung compliance refers to the ability of the lungs to expand and contract in response to changes in pressure. High compliance means the lungs can easily expand with minimal pressure, while low compliance indicates stiff lungs that require higher pressures to inflate [19].
Pplat and Lung Compliance
Maintaining a Pplat below 30 cmH2O is essential to prevent ventilator-induced lung injury [20]. Elevated Pplat suggests poor lung compliance, which may be due to conditions such as acute respiratory distress syndrome (ARDS) or pulmonary fibrosis [21]. By monitoring and adjusting Pplat, clinicians can optimize ventilatory support and minimize the risk of lung injury [22].
Interrelation
- High PIP with Normal Pplat: This indicates an increased airway resistance without a problem in lung or chest wall compliance. This situation often suggests an obstruction within the airway, such as:
- Bronchospasm (as seen in asthma or COPD) [23].
- Mucus plugging [24].
- Kinked endotracheal tube [25].
- High PIP with High Pplat: This suggests a problem with lung compliance rather than just airway resistance. Both PIP and Pplat are elevated, indicating that the lungs or chest wall are stiffer or less compliant. Conditions associated with this pattern include:
- Pulmonary edema [26].
- Acute Respiratory Distress Syndrome (ARDS) [27].
- Pulmonary fibrosis [28].
- Pneumothorax (collapsed lung) [29].
- Atelectasis (collapse of lung tissue) [30].
Conclusion
Understanding and managing PEEP, PIP, and Pplat are fundamental to the effective use of mechanical ventilation. These parameters ensure that the patient’s lungs are ventilated safely and efficiently, reducing the risk of lung injury and improving overall outcomes [31]. Healthcare providers must have a thorough understanding of these principles to provide the best care for their patients [32].
References:
- Tobin MJ. Principles and Practice of Mechanical Ventilation. McGraw Hill; 2013.
- Guyton AC, Hall JE. Textbook of Medical Physiology. 12th ed. Elsevier Saunders; 2011.
- Marini JJ, Wheeler AP. Critical Care Medicine: The Essentials. Lippincott Williams & Wilkins; 2012.
- Hess DR, MacIntyre NR. Essentials of Mechanical Ventilation. McGraw Hill; 2021.
- Pilbeam SP. Mechanical Ventilation: Physiological and Clinical Applications. 6th ed. Elsevier; 2021.
- Kacmarek RM, Stoller JK, Heuer AJ. Egan’s Fundamentals of Respiratory Care. Elsevier; 2020.
- Brochard L, Slutsky A, Pesenti A. Mechanical Ventilation to Minimize Progression of Lung Injury in Acute Respiratory Failure. Am J Respir Crit Care Med. 2017;195(4):438-442.
- Brower RG, Matthay MA, Schoenfeld D, et al. The Acute Respiratory Distress Syndrome Network. NEJM. 2000;342(18):1301-1308.
- Chatburn RL. Fundamentals of Mechanical Ventilation: Principles and Practice. Springer; 2019.
- Laffey JG, Bellani G, Pham T, et al. Mechanical Ventilation in ARDS: A State-of-the-Art Review. Crit Care Med. 2017;45(8):1357-1364.
- Kallet RH. Ventilator Management Strategies for Obstructive Lung Disease in Acute Respiratory Failure. Respir Care. 2019;64(6):788-807.
- Slutsky AS, Ranieri VM. Ventilator-Induced Lung Injury. NEJM. 2013;369:2126-2136.
- Dreyfuss D, Saumon G. Barotrauma is Volutrauma, but which is worse? Intensive Care Med. 1992;18(3):139-141.
- ARDSNet Study. Ventilation with Lower Tidal Volumes as Compared with Traditional Tidal Volumes for Acute Lung Injury and the Acute Respiratory Distress Syndrome. NEJM. 2000;342:1301-1308.
- Tobin MJ. Respiratory Monitoring in the ICU. In: Principles and Practice of Intensive Care Monitoring. Springer; 1997.
- Hubmayr RD. Mechanical Ventilation of Acute Respiratory Failure: General Approach. UpToDate. Accessed October 10, 2023.
- McConville JF, Kress JP. Weaning Patients from the Ventilator. NEJM. 2012;367:2233-2239.
- Beitler JR, Malhotra A, Thompson BT. Ventilator-Induced Lung Injury. Clin Chest Med. 2016;37(4):633-646.
- Tobin MJ. Mechanical Ventilation and Bronchospasm. Chest. 1992;101(3):336-337.
- Sassoon CSH. Ventilator-Associated Mucus Plugging: Prevention and Treatment. Respir Care. 2011;56(10):1410-1413.
- Wilkins RL, Stoller JK, Scanlan CL. Egan’s Fundamentals of Respiratory Care. Elsevier Saunders; 2013.
- ARDSNet Study. Ventilator-Induced Lung Injury in ARDS. NEJM. 1999;341:1964-1967.
- Kallet RH, Alonso JA, Diaz AA. Effects of Mechanical Ventilation on ARDS. Respir Care. 2013;58(9):1600-1606.
- Matamis D, Lemaire F, Harf A, et al. Flow-Volume Curves and Pressure-Volume Loops in the Monitoring of Acute Respiratory Failure. Intensive Care Med. 1984;10(3):121-127.
- Tobin MJ. Principles and Practice of Mechanical Ventilation. McGraw Hill; 2006.
- Slutsky AS, Ranieri VM. Ventilator-Induced Lung Injury. NEJM. 2013;369:2126-2136.
- Hess DR. Ventilator-Induced Lung Injury: Mechanisms, Management, and Prevention. Respir Care. 2013;58(5):789-801.