In the high-stakes world of critical care medicine, healthcare providers are constantly faced with the challenge of managing patients with unstable blood pressure. Two key classes of medications often come into play in these situations: pressors and inotropes. While both serve the crucial purpose of supporting blood pressure, it’s essential to understand the distinctions between these pharmacological interventions to optimize patient care.
Pressors: Raising the Bar on Blood Pressure
Pressors, short for vasopressors, are a class of medications primarily focused on increasing systemic vascular resistance. These drugs act by constricting blood vessels, thereby raising blood pressure. In critical care scenarios, pressors are often employed to counteract severe hypotension, which can be life-threatening.
Common examples of pressors include norepinephrine, epinephrine, and phenylephrine. Norepinephrine, for instance, is frequently used to address distributive shock, such as septic shock, by tightening blood vessels and boosting blood pressure. These medications play a vital role in stabilizing patients in critical conditions where maintaining adequate perfusion is paramount.
Inotropes: Enhancing Cardiac Performance
On the other hand, inotropes primarily focus on enhancing the force of cardiac contractions. These medications come into play when the heart’s pumping ability is compromised, leading to a decrease in cardiac output. Inotropes positively impact the contractility of the heart muscle, ensuring an adequate supply of blood to vital organs.
Dobutamine and milrinone are commonly used inotropes. Dobutamine, for example, is employed to support patients with heart failure or those recovering from cardiac surgery, where a boost in cardiac contractility is essential. By optimizing the heart’s performance, inotropes contribute to maintaining adequate cardiac output and organ perfusion.
The Delicate Balance: Pressors vs. Inotropes
Understanding the nuanced differences between pressors and inotropes is crucial for healthcare providers navigating the complexities of critical care. While both classes of medications aim to support blood pressure, their mechanisms of action and targeted physiological systems differ significantly.
Pressors target vascular resistance, ensuring blood vessels remain constricted to elevate blood pressure. In contrast, inotropes focus on the heart’s contractility, enhancing its ability to pump blood efficiently. The choice between these interventions depends on the underlying cause of the patient’s hemodynamic instability.
The Symphony of Patient Management
In critical care, the orchestration of patient management often involves a delicate balance between pressors and inotropes. Healthcare providers must carefully assess the patient’s condition, considering factors such as the cause of hemodynamic instability, cardiac function, and overall perfusion.
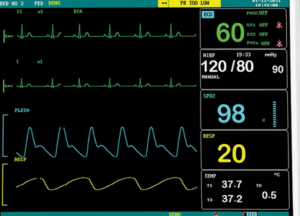
It is crucial for healthcare providers to remain vigilant in monitoring patients receiving these medications, as inappropriate or excessive use can lead to adverse effects. Regular assessment of blood pressure, heart rate, and organ perfusion is essential to ensure the optimal dosage and duration of therapy.
Conclusion: Knowing the Difference Matters
In the realm of critical care, the distinction between pressors and inotropes is more than just semantics; it’s a critical component of providing effective patient care. Navigating the complexities of hemodynamic management requires a nuanced understanding of these pharmacological interventions.
Healthcare providers play a pivotal role in maintaining this delicate balance, ensuring that patients receive the right medication for their specific needs. As we continue to advance in the field of critical care medicine, it remains paramount for healthcare professionals to deepen their knowledge of pressors and inotropes, recognizing their distinct roles in the management of critically ill patients. In doing so, we empower ourselves to deliver the highest standard of care and safeguard the well-being of those entrusted to us.