Throughout my career, I’ve adhered to a fundamental principle: treat the patient, not the monitor or device. This approach emphasizes the importance of holistic patient assessment, where clinical judgment takes precedence over numerical readings. While pulse oximetry remains a valuable tool, it is but one piece of the diagnostic puzzle.
Understanding the Challenge:
Pulse oximetry, a crucial diagnostic tool, offers insights into blood oxygen saturation levels, but its accuracy can be influenced by various factors. What do I mean? In order to understand this, we need to understand how SpO2 is measured or in other words the technical side of things.
The Science Behind SpO2:
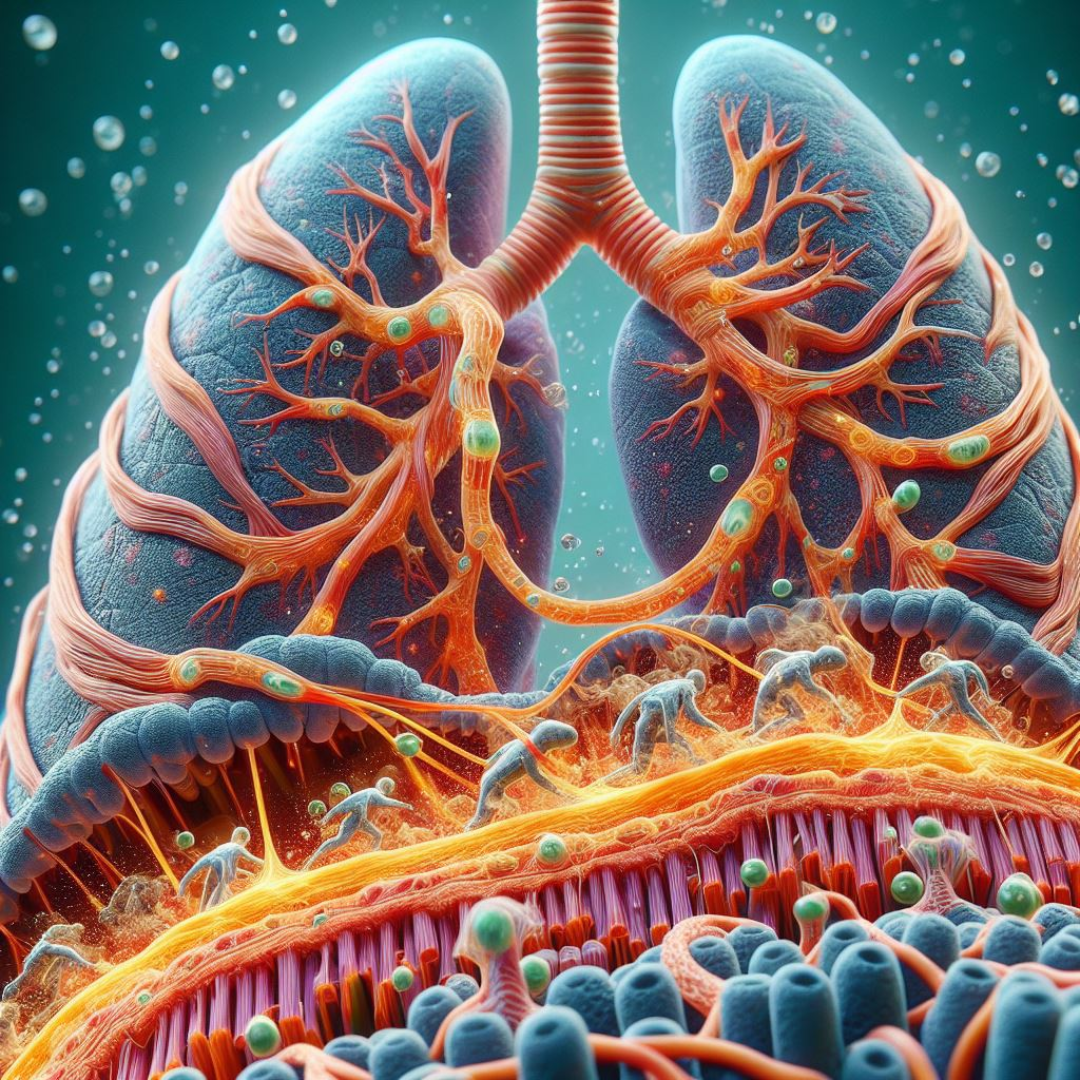
Pulse oximetry operates on the principle of spectrophotometry, using light wavelengths to detect the proportion of oxygenated hemoglobin in the blood. While this technology has revolutionized patient care, studies have uncovered some concerning trends.
Firstly:
Pulse oximeters may yield inaccurate readings in individuals with darker skin tones. The discrepancy arises from differences in skin pigmentation. Melanin, the pigment responsible for skin color, absorbs light, particularly in the red and infrared spectrum used by pulse oximeters, a phenomenon called “perfusion index.” As a result, the device may overestimate oxygen saturation levels in individuals with darker skin tones, potentially masking underlying hypoxemia.
Secondly: Pulse oximetry, while offering a snapshot of oxygen saturation levels in the blood, it’s crucial to recognize that this measurement presents a retrospective view, capturing the state of oxygen diffusion across lung membranes about 1-2 minutes prior to the reading. Therefore, it’s important to understand that the information provided is retrospective in nature, offering a glimpse into the past rather than an immediate snapshot. Additionally, this retrospective view is influenced by various physiological factors, including the volume of blood in the body, stroke volume, heart rate, and the dynamics of blood circulation.
Let’s consider the volume of blood circulating in the body. The human body contains approximately 5-6 liters of blood, which continuously circulates to deliver oxygen to tissues and remove carbon dioxide. This circulation involves the heart pumping blood out to the body through arteries and then returning it to the heart via veins. However, this process takes time, as blood travels through the circulatory system.
Now let’s consider the stroke volume, which refers to the amount of blood pumped out of the heart with each contraction, and the heart rate, which denotes the number of times the heart beats per minute, both are vital factors influencing blood circulation. Together, they determine the rate at which oxygenated blood is delivered to tissues and deoxygenated blood returns to the heart and lungs for reoxygenation.
Moreover, the journey of blood from the lungs, where oxygen is taken up and carbon dioxide is released, to the peripheral tissues, and back to the heart, involves a certain time delay. This delay is influenced by factors such as the distance between the lungs and the peripheral tissues, the efficiency of oxygen uptake and release, the diameter of the vasculature and, the speed of blood flow through the vessels.
As a result, when pulse oximetry measures oxygen saturation levels, it reflects the state of oxygen diffusion across lung membranes approximately 1-2 minutes prior to the reading. This delay accounts for the time it takes for blood to travel from the lungs to the peripheral tissues and back again, as well as the time required for oxygen to move across the alveolar-capillary membrane in the lungs and bind to hemoglobin.
In essence, while pulse oximetry provides valuable information about oxygen saturation levels, it’s essential to interpret these readings within the context of the patient’s overall clinical condition and the dynamics of blood circulation. Through critical thinking and understanding the perfusion index and the retrospective nature of pulse oximetry, healthcare professionals can make better clinical decisions and provide optimal care to their patients
Treating the Patient, Not Just the Device Reading:
It’s important for paramedics and healthcare providers to recognize the limitations of pulse oximetry, especially in emergency situations where timely interventions are crucial, reliance on inaccurate pulse oximetry readings can lead to misdiagnosis and inappropriate treatment decisions. While pulse oximetry remains a valuable tool, it should not be relied upon as the sole indicator of a patient’s oxygenation status.
Instead, healthcare professionals should prioritize a holistic approach to patient care, taking into account clinical symptoms, medical history, and physical examination findings in addition to pulse oximetry readings. It is imperative that we adopt a patient-centered approach to care. While pulse oximetry remains a valuable tool, it should complement, not replace, comprehensive clinical assessment. If a patient exhibits signs of shortness of breath, hypoxia, or respiratory distress, prompt intervention and treatment are paramount, regardless of the oxygen saturation readings displayed on the pulse oximeter.