Introduction
Hospital-acquired pneumonia (HAP) remains a significant concern in healthcare settings, especially among critically ill patients. It is defined as pneumonia that occurs 48 hours or more after admission, which was not incubating at the time of admission. Ventilator-associated pneumonia (VAP), a subset of HAP, particularly affects patients receiving mechanical ventilation. This article explores the pathobiology, complications, and preventive strategies for HAP, with a focus on the critical role of healthcare workers in prevention.
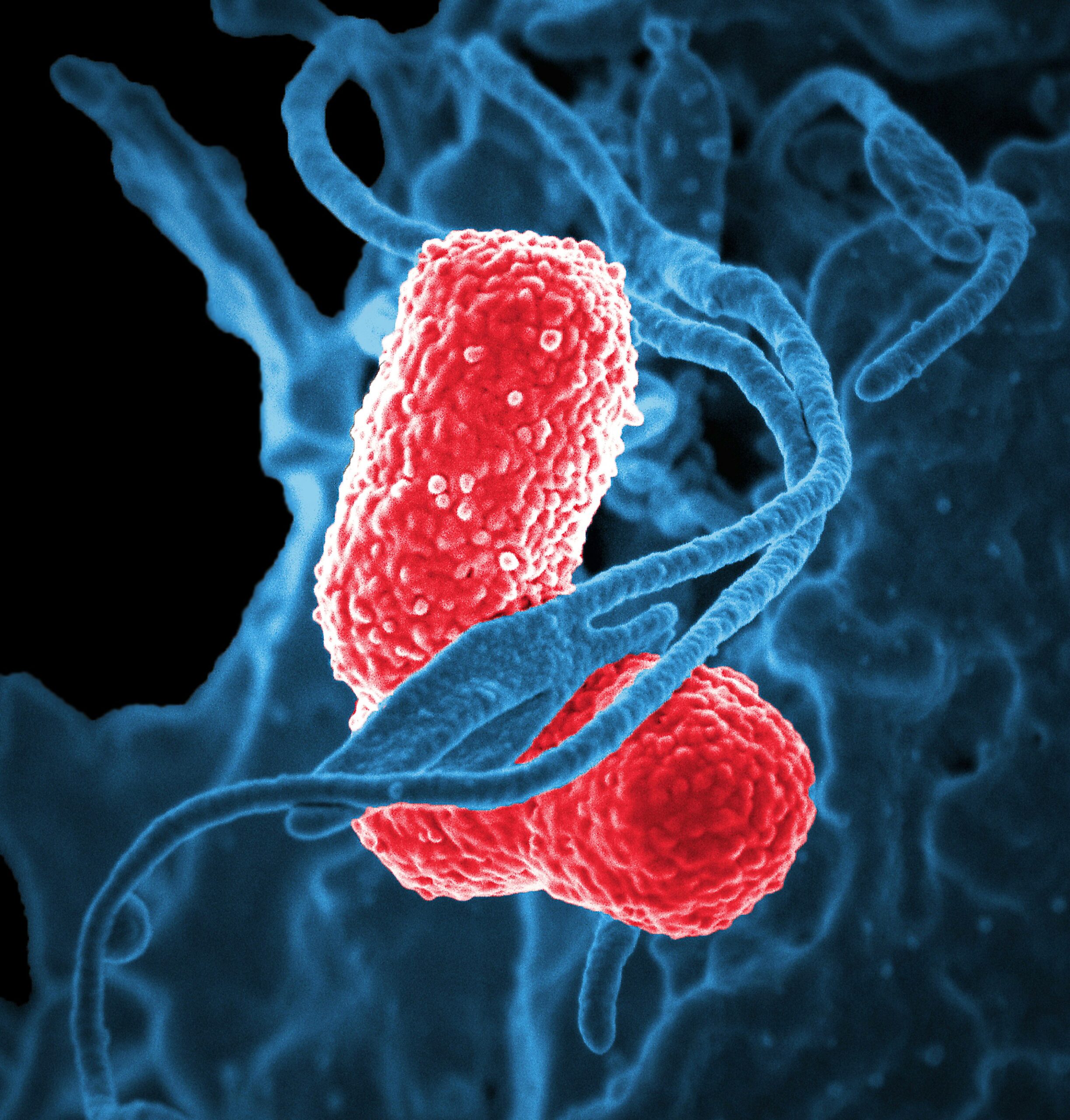
Understanding HAP and VAP
HAP is a leading cause of infection-related mortality in hospitals. VAP, which develops in 20-36% of patients on mechanical ventilation, poses a severe threat due to its high morbidity and mortality rates [1]. The risk factors for HAP include prolonged hospital stay, mechanical ventilation, immunosuppression, and previous antibiotic use [2].
Pre-Hospital Intubations and HAP Incidence
Pre-hospital intubation, often performed by emergency medical services (EMS), is an essential intervention for patients requiring immediate airway management. However, it has been associated with an increased risk of developing HAP. The reasons for this include::
- Suboptimal Conditions: Pre-hospital intubations are frequently performed in less-than-ideal conditions, such as in ambulances or at the scene of an accident, which can increase the risk of contamination and subsequent infection [3].
- Delayed Care: Patients intubated pre-hospital may experience delays in receiving appropriate antibiotics and other medical interventions, increasing the risk of infection [3].
- Increased Aspiration Risk: The urgent nature of pre-hospital intubations can lead to a higher risk of aspiration, contributing to the development of pneumonia [3].
Studies have shown that patients who undergo pre-hospital intubation have a higher incidence of HAP compared to those intubated within the controlled environment of a hospital [3]. This highlights the need for improved training and protocols for EMS personnel to minimize infection risks.
Complications of HAP
The complications associated with HAP are numerous and severe. They include:
- Increased Mortality: Mortality rates for HAP, particularly VAP, range from 24% to 76% [1].
- Septic Shock: Delayed or inappropriate treatment can lead to septic shock, a life-threatening condition.
- Acute Respiratory Distress Syndrome (ARDS): HAP can cause ARDS, further complicating the patient’s condition and increasing mortality risk.
- Antibiotic Resistance: The high antibiotic pressure from treating HAP leads to the development of multidrug-resistant (MDR) pathogens [4].
- Prolonged Hospital Stay and Increased Costs: HAP extends hospital stays by an average of four to nine days, significantly increasing healthcare costs [1].
Preventing HAP
Prevention of HAP is crucial and can be achieved through several strategies:
- Infection Control Measures: Rigorous hand hygiene, use of personal protective equipment, and sterilization protocols are essential.
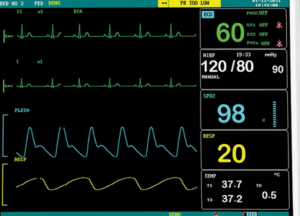
- Ventilator Care Bundle: Implementing a bundle of care practices for patients on mechanical ventilation can reduce the incidence of VAP. This includes elevating the head of the bed, daily sedation vacations, and assessment of readiness to extubate, peptic ulcer disease prophylaxis, and deep venous thrombosis prophylaxis [1].
- Oral Care: Regular oral care with antiseptics like chlorhexidine can reduce the risk of bacterial colonization in the oropharynx, a common source of HAP [5].
- Antibiotic Stewardship: Judicious use of antibiotics to avoid overuse and resistance development is critical. This includes de-escalation based on culture results and using the shortest effective course of therapy [4].
- Early Mobilization: Encouraging early mobilization of patients can help improve lung function and reduce the risk of pneumonia [6].
- Continuous Education and Training: Regular training for healthcare workers on infection control practices and updates on new preventive measures is vital [7].
Impact on Patients
The impact of HAP on patients is profound, leading to increased morbidity, extended hospital stays, and higher healthcare costs. Patients suffer from prolonged discomfort, increased risk of complications, and a higher likelihood of mortality. Additionally, the psychological impact on patients and their families due to extended hospitalization and severe illness cannot be underestimated [1].
Call to Action for Healthcare Workers
Preventing HAP requires a coordinated effort from all healthcare workers. Here are key actions healthcare professionals can take:
- Adhere to Infection Control Practices: Consistently follow hand hygiene protocols and use appropriate personal protective equipment.
- Implement and Follow Care Bundles: Strictly adhere to ventilator care bundles and other preventive protocols.
- Educate and Train: Participate in regular training sessions and stay updated on best practices and new guidelines.
- Promote Antibiotic Stewardship: Use antibiotics judiciously and support policies that promote the responsible use of antibiotics.
- Encourage Patient Mobility: Facilitate and encourage early mobilization of patients whenever possible.
- Engage in Continuous Improvement: Regularly review and improve infection prevention protocols based on the latest evidence and guidelines.
Conclusion
HAP is a significant cause of morbidity and mortality in hospitalized patients, especially those in critical care. By understanding its complications and implementing robust preventive strategies, healthcare workers can significantly reduce its incidence and impact. Continuous education, adherence to infection control practices, and a collaborative approach are essential in the fight against HAP. Let us commit to these actions to improve patient outcomes and enhance the quality of care in our healthcare facilities.
References
- Howroyd, F., Chacko, C., MacDuff, A., Gautam, N., Pouchet, B., Tunnicliffe, B., Weblin, J., Gao-Smith, F., Ahmed, Z., Duggal, N. A., & Veenith, T. (2024). Ventilator-associated pneumonia: pathobiological heterogeneity and diagnostic challenges. Nature Communications, 15, 6447.
- Barbier, F., Andremont, A., Wolff, M., & Bouadma, L. (2013). Hospital-acquired pneumonia and ventilator-associated pneumonia: recent advances in epidemiology and management. Current Opinion in Pulmonary Medicine, 19(3), 216–228.
- Chastre, J., & Fagon, J. Y. (2002). Ventilator-associated pneumonia. American Journal of Respiratory and Critical Care Medicine, 165(7), 867-903.
- Rotstein, C., Evans, G., Born, A., Grossman, R., Light, R. B., Magder, S., McTaggart, B., Weiss, K., & Zhanel, G. G. (2008). Clinical practice guidelines for hospital-acquired pneumonia and ventilator-associated pneumonia in adults. Canadian Journal of Infectious Diseases and Medical Microbiology, 19(1), 19-53.
- Jackson, L., & Owens, M. (2019). Does oral care with chlorhexidine reduce ventilator-associated pneumonia in mechanically ventilated adults? British Journal of Nursing, 28(11), 682-689.
- Masterton, R. G., Galloway, A., French, G., Street, M., Armstrong, J., Brown, E., … & Watson, A. (2008). Guidelines for the management of hospital-acquired pneumonia in the UK: report of the working party on hospital-acquired pneumonia of the British Society for Antimicrobial Chemotherapy. Journal of Antimicrobial Chemotherapy, 62(1), 5-34.
- Kalil, A. C., Metersky, M. L., Klompas, M., Muscedere, J., Sweeney, D. A., Palmer, L. B., … & Brozek, J. L. (2016). Management of adults with hospital-acquired and ventilator-associated pneumonia: 2016 clinical practice guidelines by the Infectious Diseases Society of America and the American Thoracic Society. Clinical Infectious Diseases, 63(5), e61-e111.



Great blog! Is your theme custom made or did you download
it from somewhere? A design like yours with a few simple tweeks would really make
my blog stand out. Please let me know where
you got your design. Thank you
Great article.
Hello there, You have done an excellent job. I’ll certainly digg it and personally suggest to my friends. I’m sure they will be benefited from this website.
I used to be able to find good info from your articles.
I blog frequently and I truly thank you for your content.
This article has really peaked my interest. I’m going to book mark your site and keep checking for new information about once per week.
I opted in for your Feed as well.
Excellent site you have got here.. It’s difficult to find
high-quality writing like yours these days. I truly appreciate individuals like you!
Take care!!
Excellent goods from you, man. I have understand your stuff previous to and you’re just extremely fantastic.
I actually like what you have acquired here, certainly like what you’re stating and the way
in which you say it. You make it enjoyable and you still care for to keep it wise.
I can’t wait to read much more from you. This is really a tremendous site.
Peculiar article, just what I wanted to find.
Hey! Someone in my Facebook group shared this website with us so I came to take a look.
I’m definitely enjoying the information. I’m bookmarking and will
be tweeting this to my followers! Outstanding blog and
fantastic design and style.
I was able to find good advice from your blog posts.
Howdy! This post could not be written much better! Going through this article reminds me of my previous roommate!
He constantly kept talking about this. I’ll forward this post to him.
Pretty sure he’ll have a good read. Many thanks for sharing!