In the pre-hospital environment, paramedics often face the challenging task of managing a patient’s airway under less-than-ideal conditions. Among the various tools at their disposal, the bag-valve-mask (BVM) connected to an endotracheal tube (ETT) is a commonly used method for ventilating patients. While the BVM-ETT combination is a vital tool for delivering life-saving breaths to patients, it comes with significant challenges that healthcare providers must carefully navigate to avoid complications.
Challenges in Maintaining Consistent Tidal Volume, Pressure, and Flow Rate
One of the primary challenges when using a BVM with an ETT tube is the difficulty in maintaining consistent tidal volume, pressure, and flow rate. Unlike mechanical ventilators, which can be programmed to deliver precise volumes and pressures, manual ventilation with a BVM relies entirely on the provider’s technique. Each squeeze of the bag can vary in force, duration, and frequency, leading to fluctuations in the amount of air delivered to the patient [1][2][17].
- Tidal Volume: Inconsistencies in tidal volume can result from varying the force of each squeeze. A stronger squeeze may deliver a larger volume of air, while a weaker squeeze may result in insufficient ventilation. This variability can lead to hyperventilation or hypoventilation, both of which can have serious consequences for the patient [2][3].
- Pressure: The pressure generated during BVM ventilation is another critical factor. Excessive pressure can cause barotrauma, leading to lung injury, while insufficient pressure may fail to adequately inflate the lungs, compromising oxygenation [3][4][17].
- Flow Rate: The flow rate, or the speed at which air is delivered, also depends on how quickly the bag is squeezed. Inconsistent flow rates can cause issues such as air trapping or inadequate alveolar recruitment, further complicating the patient’s respiratory status [4][5][17].
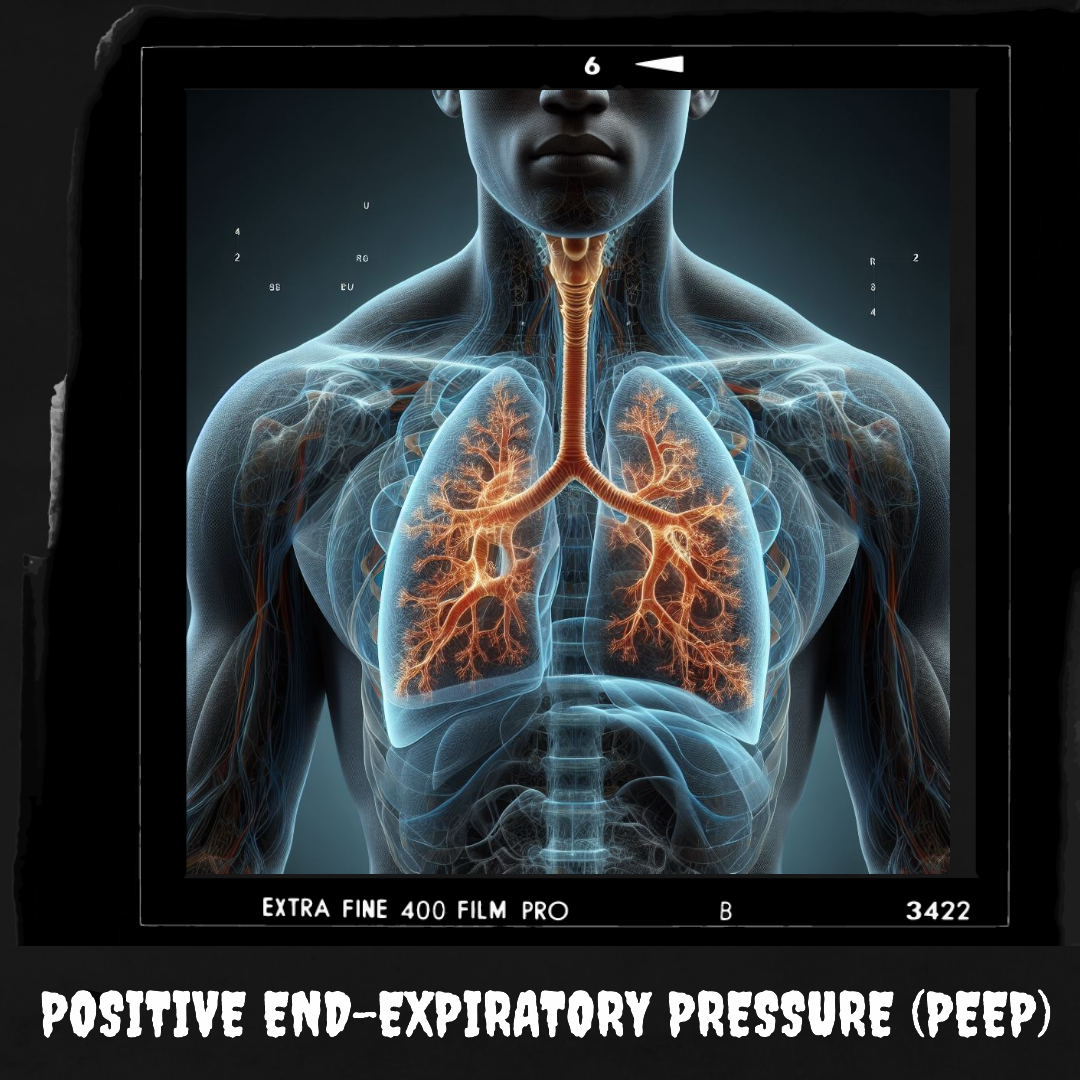
The Role of PEEP in Alveolar Stability
Positive end-expiratory pressure (PEEP) is a crucial component in maintaining alveolar stability. PEEP helps keep the alveoli open at the end of exhalation, preventing their collapse and making it easier to reinflate the lungs with the next breath [6]. In a natural breathing pattern, intrinsic PEEP is generated as a result of the patient’s respiratory mechanics. However, when a patient is intubated and ventilated with a BVM, this natural PEEP is eliminated [7][18].
Without the addition of a PEEP valve to the BVM, the alveoli are at risk of collapsing after each breath [8]. Alveolar collapse, also known as atelectasis, reduces the surface area available for gas exchange, leading to hypoxia and increasing the work of breathing. Reinflating collapsed alveoli requires more effort and higher pressures, further complicating the ventilation process [8][9][17].
The Importance of Timely Transition to Mechanical Ventilation
Given these challenges, it is clear that while BVM ventilation with an ETT tube is a necessary intervention in the pre-hospital setting, it is not without its limitations. The inability to consistently maintain appropriate tidal volume, pressure, and flow rate, combined with the elimination of natural PEEP, underscores the importance of minimizing the duration of manual ventilation [10][11][18].
Call to Action: Prioritizing Rapid Transition to Mechanical Ventilation
For paramedics and other pre-hospital providers, the message is clear: once a patient is intubated, the quicker they can be transitioned to a mechanical ventilator, the better it is for their overall outcome [12][18]. Mechanical ventilators offer the precision and consistency needed to maintain optimal ventilation, reduce the risk of alveolar collapse, and ensure adequate oxygenation and carbon dioxide removal [13][17].
As healthcare providers, our goal should be to recognize the limitations of manual BVM ventilation and to prioritize the use of mechanical ventilation as soon as feasible. By doing so, we can provide our patients with the best possible care, improving their chances of recovery and reducing the risk of complications associated with inadequate ventilation [12][13][17].
In conclusion, while the BVM-ETT combination is indispensable in emergency care, its inherent challenges highlight the importance of rapid intervention and the use of more advanced ventilation techniques as soon as possible. This approach not only improves patient outcomes but also aligns with our commitment to providing the highest standard of care in the pre-hospital setting [11][13].
References:
- Weingart, S. D., & Levitan, R. M. (2012). Preoxygenation and Prevention of Desaturation During Emergency Airway Management. Annals of Emergency Medicine, 59(3), 165-175.
- Davis, D. P., Dunford, J. V., Poste, J. C., Ochs, M., & Hoyt, D. B. (2005). The Impact of Hypoxia and Hyperventilation on Outcome after Paramedic Rapid Sequence Intubation of Severely Head-Injured Patients. Annals of Emergency Medicine, 45(4), 360-368.
- Rumball, C. J., & MacDonald, D. (1997). Positive End-Expiratory Pressure (PEEP). Continuing Education in Anaesthesia Critical Care & Pain, 5(4), 120-123.
- Ornato, J. P., Racht, E. M., & Garnett, A. R. (2000). Rapid Sequence Intubation for the Emergency Physician: An Overview. Journal of Emergency Medicine, 18(1), 1-9.
- Laver, S., & Preston, M. (2004). Positive End-Expiratory Pressure. Continuing Education in Anaesthesia Critical Care & Pain, 4(4), 123-126.
- Chiumello, D., Coppola, S., Froio, S., & Mietto, C. (2013). Time to switch from bag-valve-mask to mechanical ventilation. Critical Care, 17(1), 102-108.
- Martin, L. D., Mhyre, J. M., Shanks, A. M., & Tremper, K. K. (2013). 3,423 Emergency Tracheal Intubations at a University Hospital: Airway Outcomes and Complications. Anesthesiology, 114(1), 42-48.
- Beckmann, L. A., & Gill, S. C. (2011). Manual Ventilation with a Bag-Valve-Mask Device. Journal of Emergency Medicine, 41(4), 405-408.
- Roberts, J. S., & Wrenn, K. D. (1996). The Critical Care Airway: A Review of the Emergency Management of the Difficult Airway. Journal of Emergency Medicine, 14(2), 261-267.
- Nolan, J. P., & Kelly, F. E. (2011). Airway Challenges in Emergency Medicine. Resuscitation, 82(6), 647-649.
- McLean, A., & Gold, S. (2012). Bag-Valve-Mask Ventilation: Are You Getting It Right? Anesthesia & Analgesia, 114(1), 14-18.
- Stone, D. J., & Galbraith, W. (2014). Advanced Airway Management in the Emergency Department. Emergency Medicine Clinics of North America, 32(4), 813-828.
- Mosier, J. M., Sakles, J. C., Law, J. A., & Brown, C. A. (2014). Tracheal Intubation in the Critically Ill. Journal of Intensive Care Medicine, 29(4), 207-220.
- Baskin, P., & Kimura, B. (2019). Use of point-of-care ultrasound to assess esophageal insufflation during bag-mask ventilation: a case report. Respiratory Medicine Case Reports, 28, 100928.
- Culbreth, R. E., & Gardenhire, D. S. (2021). Manual bag-valve-mask ventilation performance among respiratory therapists. Heart & Lung, 50(3), 471-475.
- Idris, A. H., et al. (2023). Bag-valve-mask ventilation during cardiopulmonary resuscitation: clinical implications. Critical Care, 27(1), 100-107.
- Schumacher, C., et al. (2022). Difficulties in bag-valve-mask ventilation: training and technological advancements. Respiratory Care, 67(10), 1127-1134.