Extracorporeal Membrane Oxygenation (ECMO) is a sophisticated medical technology that provides life-saving support to patients with severe heart and lung conditions. Think of ECMO as a machine that temporarily takes over the work of the heart and lungs, allowing these vital organs to rest and heal. This article will break down ECMO into simple terms, explain how it works, the different types available, how it’s used in medical practice, potential complications, and considerations for patient transfers.
What is ECMO?
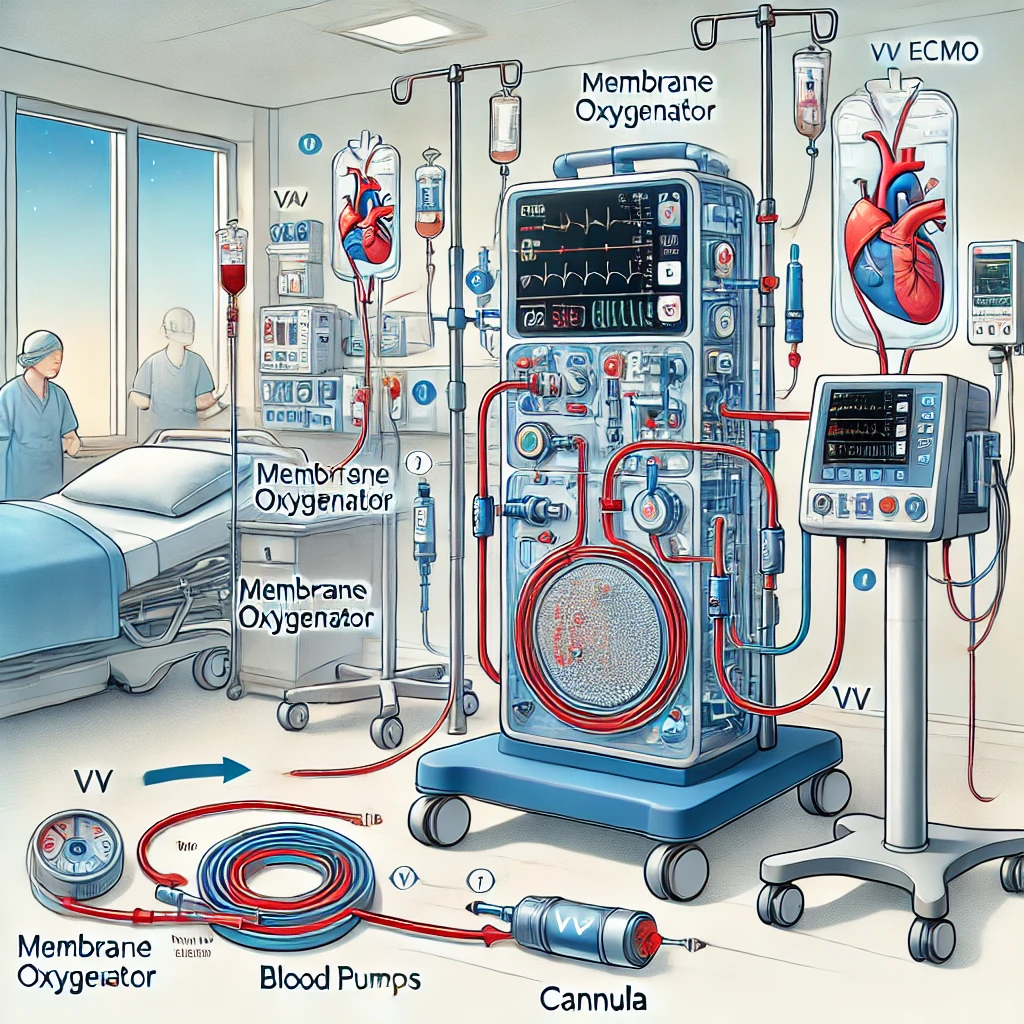
ECMO stands for Extracorporeal Membrane Oxygenation. It is a form of life support that uses a machine to oxygenate a patient’s blood outside their body and then pump it back in. Essentially, it serves as an artificial heart and lung for patients whose own organs are failing and need time to recover.
Here’s a more detailed breakdown of what ECMO does:
- Extracorporeal: This term means “outside the body.” ECMO involves taking the blood out of the body to treat it.
- Membrane: Refers to the membrane oxygenator, a component of the ECMO machine that acts like an artificial lung.
- Oxygenation: The process of adding oxygen to the blood and removing carbon dioxide, mimicking what healthy lungs do.
How Does ECMO Work?
The ECMO process involves several key steps:
- Blood Removal: Blood is drawn from a large vein or artery in the patient’s body using a cannula (a flexible tube). For VA ECMO, this usually means drawing blood from a vein and returning it to an artery, while for VV ECMO, blood is drawn and returned to veins.
- Oxygenation and Carbon Dioxide Removal: This is the core function of ECMO. Here’s a detailed look at how it happens:
- Oxygenation: The blood passes through a device called the membrane oxygenator. Inside this device, the blood flows over a thin, gas-permeable membrane. On one side of the membrane is the blood, and on the other side, a gas mixture (usually rich in oxygen and devoid of carbon dioxide) is pumped. Oxygen diffuses across the membrane into the blood because of the high concentration gradient, just as it would in the lungs.
- Carbon Dioxide Removal: Simultaneously, carbon dioxide from the blood diffuses out across the membrane into the gas mixture on the other side, which is then expelled. This mimics the gas exchange process that happens in the alveoli of healthy lungs.
- Blood Return: The oxygen-rich blood is then pumped back into the patient’s body through another vein or artery, completing the cycle.
Types of ECMO
There are two main types of ECMO, each suited for different medical conditions:
- Veno-Arterial (VA) ECMO:
- Purpose: Supports both heart and lung function.
- Procedure: Blood is taken from a vein (often the femoral vein) and returned to an artery (usually the femoral artery).
- Use Case: Ideal for patients with severe heart failure or cardiac arrest. It provides support for the heart by maintaining blood circulation and pressure.
- Complications: VA ECMO can cause complications such as bleeding, clotting, limb ischemia (restricted blood flow to limbs), and infection.
- Veno-Venous (VV) ECMO:
- Purpose: Supports only lung function.
- Procedure: Blood is taken from a vein (commonly the femoral or internal jugular vein) and returned to another vein.
- Use Case: Best for patients with severe respiratory failure but with adequate heart function. It assists in oxygenating the blood and removing carbon dioxide without directly aiding circulation.
- Complications: VV ECMO complications can include bleeding, clotting, infection, and issues with cannula placement.
Who Benefits from ECMO?
ECMO is beneficial for patients with life-threatening conditions that are not responding to conventional treatments. This includes:
- Severe Pneumonia: When traditional ventilators cannot provide sufficient oxygen.
- Acute Respiratory Distress Syndrome (ARDS): Severe lung inflammation and fluid buildup.
- Cardiogenic Shock: When the heart cannot pump enough blood to meet the body’s needs.
- Post-Cardiac Surgery: As temporary support during recovery.
- Severe Heart Failure: When other treatments have failed.
ECMO in Interfacility Transfers
Transporting a patient on ECMO between medical facilities is a complex and critical process that requires meticulous planning and coordination. Here are the key steps involved:
- Pre-Transfer Preparation:
- Stabilize the Patient: Ensure the patient is stable and the ECMO circuit is functioning correctly.
- Team Coordination: Assemble a specialized transport team including ECMO specialists, respiratory therapists, and critical care nurses and/or paramedics.
- Equipment Check: Ensure all necessary equipment, including portable ECMO machines, oxygen tanks, and medications, are ready and in working order.
- During Transfer:
- Continuous Monitoring: Constantly monitor the patient’s vital signs and the ECMO system’s performance.
- Communication: Maintain clear and constant communication between the transport team and the receiving facility.
- Post-Transfer:
- Handover: Provide a detailed handover to the receiving medical team, including the patient’s current status and any concerns that arose during transport.
- Reassessment: The receiving team will reassess the patient and make any necessary adjustments to the ECMO settings or treatment plan.
Call to Action for Paramedics
As the use of ECMO becomes more widespread, it is essential for paramedics and other prehospital care providers to have a basic understanding of this technology. Here’s why:
- Preparedness: Understanding ECMO can improve preparedness during emergencies and interfacility transfers.
- Patient Safety: Knowledge of ECMO can enhance patient safety by ensuring proper handling and monitoring during transport.
- Professional Development: Gaining ECMO knowledge is an important step in the professional development of paramedics, aligning with the evolving landscape of critical care.
I encourage all paramedics not only Critical Care and Flight Paramedics to seek out training and resources on ECMO. Whether through formal courses, online resources, or collaboration with hospitals that provide ECMO support, this knowledge can be invaluable in saving lives.
Conclusion
ECMO is a powerful tool in modern medicine, providing critical support to patients with severe heart and lung conditions. By temporarily taking over the function of these organs, ECMO allows them to rest and recover, potentially saving lives that might otherwise be lost. Understanding how ECMO works, its different types, the meticulous care required during patient transfers, and the importance of ECMO education for paramedics can help demystify this life-saving technology for everyone.
For all pre-hospital and interfacility transport providers, gaining at least a basic understanding of ECMO is crucial. It enhances preparedness, improves patient safety, and supports professional development. Let’s commit to learning more about ECMO and ensuring we are ready to provide the best care possible.
References
- Bartlett, R. H. (2007). Extracorporeal life support: history and new directions. ASAIO Journal, 53(5), 487-489.
- Brodie, D., & Bacchetta, M. (2011). Extracorporeal membrane oxygenation for ARDS in adults. New England Journal of Medicine, 365(20), 1905-1914.
- Makdisi, G., & Wang, I. W. (2015). Extra corporeal membrane oxygenation (ECMO) review of a lifesaving technology. Journal of Thoracic Disease, 7(7), E166.
- Combes, A., Brodie, D., Bartlett, R., & Brochard, L. (2014). Position paper for the organization of ECMO programs for acute respiratory failure in adult patients. American Journal of Respiratory and Critical Care Medicine, 190(5), 488-496.
- Nasr, V. G., & Thiagarajan, R. R. (2017). Transport of the extracorporeal membrane oxygenation patient. Pediatric Critical Care Medicine, 18(3_suppl), S103-S109.