What is the Shock Index?
The Shock Index (SI) is a simple, quick, and valuable tool used by healthcare professionals, especially in emergency and critical care settings, to assess the severity of a patient’s condition. It is calculated by taking the patient’s heart rate (HR) and dividing it by their systolic blood pressure (SBP). The formula is:
Shock Index (SI)=Heart Rate (HR)Systolic Blood Pressure (SBP)\text{Shock Index (SI)} = \frac{\text{Heart Rate (HR)}}{\text{Systolic Blood Pressure (SBP)}}
How is the Shock Index Measured?
To calculate the Shock Index, you need two vital signs:
- Heart Rate (HR): This is the number of times the heart beats per minute. It is typically measured using a pulse oximeter, a cardiac monitor, or by manually counting the pulse at the wrist or neck.
- Systolic Blood Pressure (SBP): This is the top number in a blood pressure reading, representing the pressure in the arteries when the heart beats. It can be measured using a blood pressure cuff (sphygmomanometer) and stethoscope, or with an automated blood pressure machine.
Once you have these two values, you divide the heart rate by the systolic blood pressure to get the Shock Index.
Interpreting the Shock Index
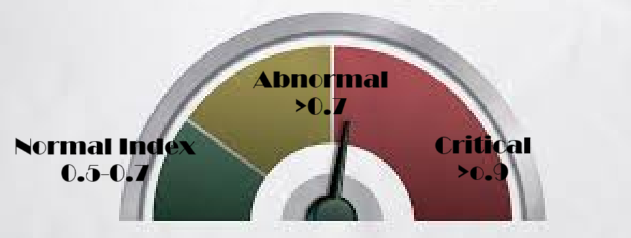
The normal range for the Shock Index in healthy individuals is generally between 0.5 and 0.7. However, certain factors, such as age, fitness level, and baseline blood pressure, can cause slight variations.
- SI < 0.5: This is considered low and might indicate a well-compensated state where the body is effectively managing its circulatory needs.
- SI between 0.5 and 0.7: This range is generally considered normal for most individuals.
- SI > 0.7: A Shock Index greater than 0.7 is concerning and may indicate that the patient is in a state of shock or is at risk of deteriorating. It suggests that the heart is working harder to maintain blood pressure, which might be a sign of circulatory failure [1].
When is the Shock Index Used?
The Shock Index is particularly useful in various clinical scenarios:
- Trauma: In trauma patients, the Shock Index can be an early indicator of hemorrhagic shock, even before significant drops in blood pressure are observed. A rising SI can signal the need for immediate interventions, such as fluid resuscitation or blood transfusion [1].
- Sepsis: In patients with sepsis, a high Shock Index may indicate that the body is struggling to maintain adequate circulation due to infection-related vasodilation and fluid shifts [3].
- Cardiogenic Shock: In cases of heart failure or myocardial infarction (heart attack), the Shock Index can help identify patients whose hearts are unable to pump effectively, leading to poor circulation and inadequate tissue perfusion [2].
- Pregnancy: During pregnancy, especially in conditions like preeclampsia, the Shock Index can help in assessing the severity of maternal health issues and guide treatment decisions [4].
What Does the Shock Index Signify?
The Shock Index is a reflection of the balance between the heart’s pumping efficiency and the resistance offered by the blood vessels. A high SI indicates that the heart is beating faster to compensate for either low blood pressure or poor circulation. This can be a sign of impending or existing shock, a life-threatening condition where the organs and tissues do not receive enough oxygen and nutrients.
Shock Index and Mortality Rate
A Shock Index greater than 0.9 is particularly concerning and is associated with a higher mortality rate in various clinical settings, including trauma and sepsis [5]. Studies have shown that patients with an SI above 0.9 are more likely to experience adverse outcomes, making it a crucial threshold in risk stratification and decision-making in emergency care [6].
In practical terms, an elevated Shock Index alerts healthcare providers to the possibility of:
- Compensated Shock: Where the body is still able to maintain adequate perfusion despite underlying issues.
- Decompensated Shock: Where the compensatory mechanisms fail, leading to a rapid decline in the patient’s condition, such as hypotension, altered mental status, and organ failure.
How to Relate to the Shock Index in Clinical Practice
In practice, the Shock Index should be considered alongside other clinical signs and symptoms, such as:
- Mental Status: Changes in consciousness or confusion can indicate inadequate brain perfusion.
- Skin Signs: Cold, clammy, or mottled skin can suggest poor circulation.
- Urine Output: Low urine output may indicate that the kidneys are not receiving enough blood, a common sign of shock.
In emergency situations, the Shock Index provides a quick and objective measure to prioritize patient care. It can be especially valuable when other more complex assessments or diagnostics are not immediately available.
Conclusion
The Shock Index is a powerful, yet simple tool that provides crucial insights into a patient’s hemodynamic status. By understanding how to measure and interpret the Shock Index, healthcare providers can make informed decisions quickly, potentially saving lives in critical situations. Always remember, however, that the Shock Index is just one piece of the puzzle and should be used in conjunction with other clinical assessments and diagnostic tools.
References
- Mutschler M, Nienaber U, Brockamp T, et al. “AIS <= 3 injuries: A better definition of blunt trauma patients at risk for complications.” J Trauma Acute Care Surg. 2014; 76(4):944-949.
- Rady MY, Smithline HA, Blake H, et al. “A comparison of the Shock Index and conventional vital signs to identify acute, critical illness in the emergency department.” Ann Emerg Med. 1994;24(4):685-690.
- Jansen TC, van Bommel J, Mulder PG, et al. “Prognostic value of blood pressure and heart rate changes in early sepsis and septic shock.” Crit Care Med. 2005;33(9):1928-1934.
- ACOG Committee Opinion No. 766: “Optimizing Postpartum Care.” Obstet Gynecol. 2019;133
.
- Cannon CM, Braxton CC, Kling-Smith M, et al. “Utility of the Shock Index in predicting mortality in trauma patients.” J Trauma. 2009;67(6):1426-1430.
- Odom SR, Howell MD, Gupta A, et al. “Extremes of Shock Index Predicts Death in Trauma Patients.” J Emerg Med. 2013;45(5):641-648.