Introduction
Hemorrhagic shock is a life-threatening condition that remains a leading cause of preventable deaths in trauma patients, particularly in the prehospital setting (1). Defined by a critical loss of circulating blood volume, it results in inadequate oxygen delivery to tissues, leading to cellular hypoxia, organ failure, and death if left untreated (2). Rapid identification and effective management of hemorrhagic shock are pivotal in improving outcomes. However, the traditional reliance on isotonic crystalloids as the primary resuscitation fluid is now under scrutiny for its limitations (3). This article explores the need for a paradigm shift toward blood-based resuscitation, addressing both the benefits and challenges, while emphasizing a call to action for prehospital providers to adopt this lifesaving approach.
The Problem with Fluid Resuscitation
For decades, isotonic crystalloids, such as normal saline or lactated Ringer’s solution, have been the standard of care for trauma patients in shock. While these fluids are widely available, inexpensive, and easy to administer, their limitations in the context of hemorrhagic shock are profound:
- Dilution of Remaining Blood
Administering large volumes of crystalloids dilutes the patient’s remaining blood, including red blood cells and clotting factors, worsening coagulopathy (1, 3). - Lack of Oxygen-Carrying Capacity
Crystalloids do not restore hemoglobin levels, leaving tissues starved of oxygen despite volume restoration (2). - Electrolyte Imbalance and Tissue Edema
Excessive use of crystalloids can lead to metabolic acidosis, tissue edema, and increased interstitial pressure, impairing oxygen and nutrient delivery (1, 4).
Evidence from recent studies suggests that excessive crystalloid administration may increase mortality in trauma patients (5). These limitations underscore the urgent need to shift from crystalloids to blood as the primary resuscitation fluid in hemorrhagic shock.
The Case for Blood-Based Resuscitation
Blood, in the form of whole blood or component therapy (packed red blood cells, plasma, and platelets), is the gold standard for replacing lost blood volume. Its advantages over crystalloids are clear:
- Oxygen Delivery
Blood transfusions immediately restore hemoglobin levels, ensuring adequate oxygen-carrying capacity and delivery to hypoxic tissues (2). - Clotting Factor Replacement
Whole blood and plasma provide essential clotting factors, reducing coagulopathy and helping to stabilize bleeding (3). - Volume Expansion Without Dilution
Blood products expand the intravascular volume without diluting clotting factors or red blood cells, unlike crystalloids (1). - Improved Patient Outcomes
Studies indicate that prehospital blood transfusion is associated with lower mortality rates, particularly in patients with profound hemorrhagic shock (4).
While blood resuscitation is clearly superior, its implementation in prehospital settings comes with logistical challenges, including storage, compatibility testing, and training. However, advancements in these areas are making prehospital blood resuscitation increasingly feasible.
Challenges and Risks of Blood Administration in the Prehospital Setting
Despite its benefits, administering blood in prehospital care presents unique challenges:
- Storage and Transport
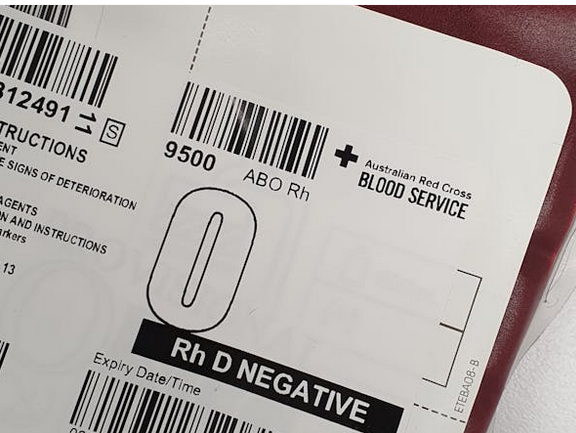
Blood products require refrigeration and have a limited shelf life. Portable refrigeration units and robust supply chains are critical to maintaining viability (4, 5). - Transfusion Reactions
Although rare with low-titer O-negative blood, adverse reactions such as febrile non-hemolytic reactions or hemolysis can occur. Prehospital providers must be trained to recognize and manage these complications (3). - Infection Control
Ensuring sterile handling of blood products in austere environments is essential to prevent infections (4). - Regulatory Barriers
Many regions require specialized certifications and protocols for prehospital blood administration, adding complexity to its adoption (5). - Cost and Resource Allocation
Blood-based resuscitation programs require significant investment in equipment, training, and coordination with blood banks (5).
Despite these challenges, the potential to save lives far outweighs the risks. A well-organized approach to logistics and training can mitigate these barriers.
The Role of Tranexamic Acid (TXA)
Tranexamic acid (TXA) is an antifibrinolytic agent that has transformed the management of hemorrhagic shock. By stabilizing clots and preventing excessive fibrinolysis, TXA reduces blood loss and improves survival when administered early in trauma care (5).
- Time-Sensitive Administration: TXA is most effective when given within the first three hours of injury. Delayed administration may reduce its efficacy and increase risks (5).
- Proven Efficacy: The CRASH-2 trial demonstrated a significant reduction in mortality with early TXA administration in trauma patients with severe hemorrhage (5).
TXA is inexpensive, easy to store, and simple to administer, making it an essential tool alongside blood transfusion in prehospital trauma care.
Recognizing Hemorrhagic Shock: Early vs. Late Signs
The ability to recognize hemorrhagic shock is critical in prehospital settings, as early intervention dramatically improves outcomes.
Early Signs
- Tachycardia and narrowed pulse pressure (1, 3)
- Pale, cool, and diaphoretic skin (1)
- Anxiety or agitation as an early indicator of hypoperfusion (1).
Late Signs
- Hypotension (a sign of decompensated shock) (3)
- Altered mental status or unconsciousness (1)
- Mottled or cyanotic skin (1)
- Oliguria or anuria, indicating severe end-organ hypoperfusion (3).
Early recognition and intervention, including the administration of TXA and blood products, are crucial to preventing the progression of shock and improving survival rates.
A Call to Action
To advance trauma care, prehospital providers and their organizations must take the following steps:
- Adopt Blood-Based Resuscitation
Implement protocols to carry low-titer O-negative whole blood or component therapy in prehospital vehicles. Collaborate with blood banks to establish reliable supply chains (4, 5). - Integrate TXA
Ensure TXA is available in all trauma response kits and train providers on its timely and appropriate use (5). - Enhance Training Programs
Conduct regular training on the recognition of hemorrhagic shock, the risks and benefits of blood administration, and the management of transfusion reactions (3). - Support Research and Policy Advocacy
Promote studies on the feasibility and impact of prehospital blood transfusion and advocate for policies that support its adoption (4). - Mitigate Logistical Challenges
Invest in portable refrigeration units, develop standardized protocols, and address regulatory hurdles to enable the safe and effective administration of blood products (4, 5).
Conclusion
Hemorrhagic shock is a time-sensitive emergency where the choice of resuscitation fluid can mean the difference between life and death. While crystalloid fluids have long been the standard of care, their limitations necessitate a shift toward blood-based resuscitation. By restoring oxygen-carrying capacity, maintaining clotting factors, and improving outcomes, blood is the optimal replacement for what trauma patients lose in hemorrhagic shock.
Despite the logistical challenges, advancements in technology, storage, and training make blood resuscitation increasingly feasible in the prehospital setting. Combined with the use of TXA, this approach represents a transformative step forward in trauma care.
Prehospital providers must advocate for the integration of blood-based resuscitation into trauma protocols. It is time to save more lives by embracing innovation, education, and the pursuit of excellence in trauma care.
References
- Cannon, J. W., et al. (2021). “Hemorrhagic shock: Advancements in understanding and management in trauma care.” Journal of Trauma and Acute Care Surgery, 91(5), 1–15.
- Spinella, P. C., et al. (2023). “Whole blood use in prehospital trauma care: A review of logistics, efficacy, and outcomes.” Prehospital Emergency Care, 27(3), 200–210.
- Shinar, Z., et al. (2022). “Prehospital blood transfusion: Best practices and emerging trends.” Critical Care Clinics, 38(4), 685–700.
- US Department of Transportation. (2023). “Prehospital Blood Transfusion Initiative Coalition: Advancing trauma care in the EMS system.” National Highway Traffic Safety Administration Report.
- CRASH-2 Trial Collaborators. (2010). “The effects of tranexamic acid on death, vascular occlusive events, and blood transfusion in trauma patients.” Lancet, 376(9734), 23–32